A person can bleed to death in minutes. University of Queensland researchers are taking inspiration from nature to develop unique hydrogels that can save people from blood loss incurred during traumatic injury.
Bleeding out from traumatic injury is a leading cause of preventable death worldwide, second only to brain and spinal cord injuries. In fact, 30-40% of civilian deaths and 90% of military mortalities are due to uncontrolled bleeding. More than half of these deaths occur before an injured person can even reach the hospital.
A first-aid kit offers little actual aid to a person in an emergency bleeding situation – place gauze on the wound and apply pressure. If the blood loss is from an arm or leg, the manual tells you to look around your surroundings and hope you find materials suitable for a tourniquet.
Easy-to-pack and easy-to-use wound treatment products are needed that effectively stop uncontrolled bleeding. Being able to treat soldiers and civilians at the point of injury has tremendous potential to save lives and reduce the mortality from traumatic injury.
Based at the Australian Institute for Bioengineering and Nanotechnology (AIBN), postdoctoral research fellow Dr Amanda Kijas and Prof. Alan Rowan have taken their cues from nature to develop novel wound management agents.
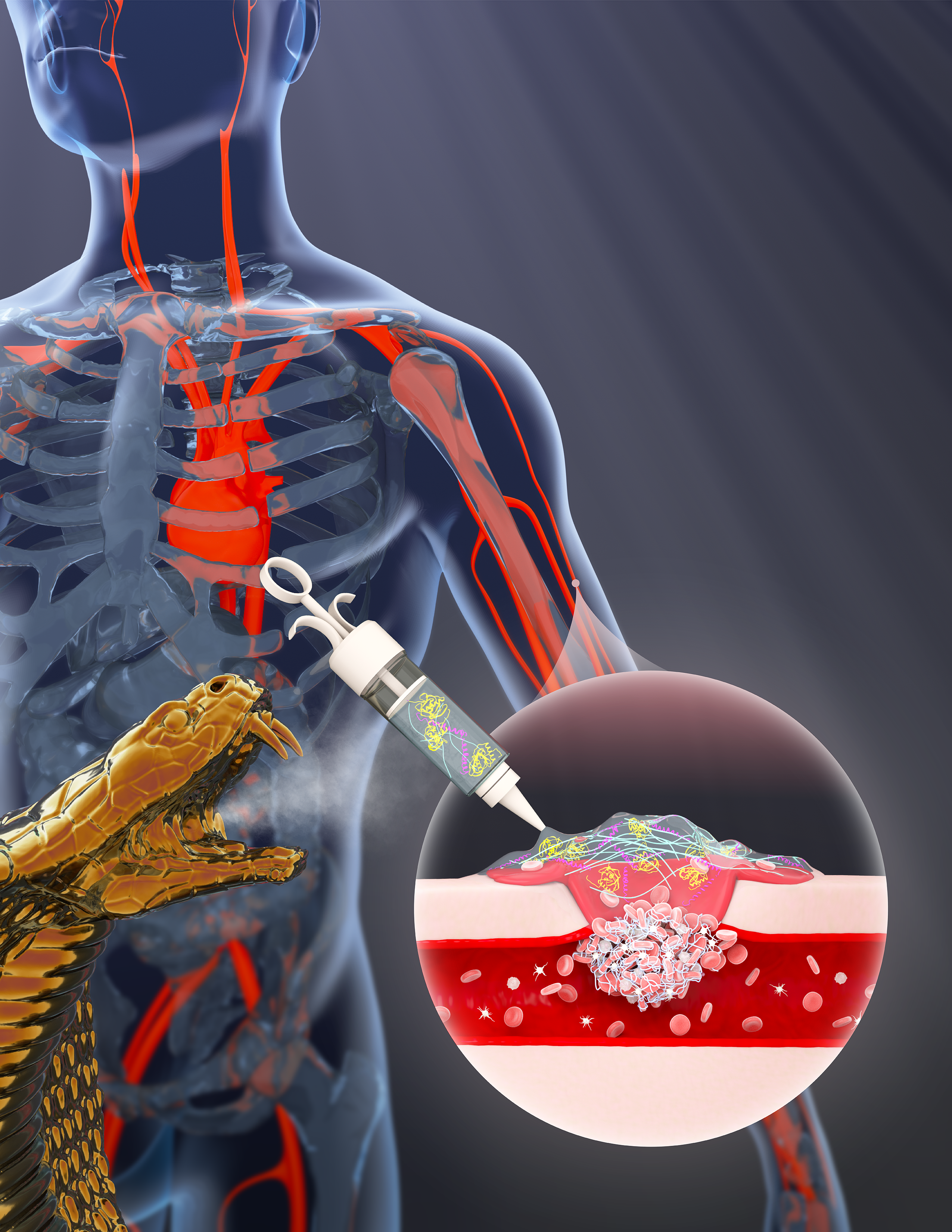
Which animal species are master manipulators of the human circulatory system? You need look no further than venomous snakes. While some compounds in venom destroy capillary vessels and cause internal bleeding, others activate the blood clotting system and block blood vessels, which can induce a stroke or heart attack.
With support from ANFF-Q facilities hosted at AIBN, the team has developed a revolutionary wound treatment system that uses potent proteins derived from venomous snakes to both accelerate clotting and retain a stable blood clot. One such snake venom protein, ecarin, begins a series of biochemical reactions that leads to the formation of fibrin, long fibres that interact with platelets to form a clot over a wound site. Overall, ecarin supercharges the clotting process and stems the flow of blood.
However, triggering clot formation within a wound is limited in effectiveness if the blood clot subsequently breaks down, a process called fibrinolysis. A major shortfall of many currently employed haemostatic (or clotting) agents is the lack of an anti-fibrinolytic agent to counter blood clot breakdown. The novel system described in this work employs a second snake venom protein called textilinin that effectively counters fibrinolysis. The addition of textilinin adds a unique capability not seen in other point-of-injury wound treatment products.
Fortunately, these venom proteins can be easily produced in the laboratory, which is much easier on both the snakes and the snake milkers. Yet, these haemostatic proteins form only part of the picture, as they need to be effectively delivered to the site of injury to have any effect. In the product, the proteins are delivered within a topically applied, thermo-responsive hydrogel to seal the wound. Below room temperature, the polymer material takes the form of a liquid. When applied to a wound, body heat warms the material, and the polymer transitions into a stable matrix similar to a jelly.
Proof-of-concept in vivo studies have demonstrated the overwhelming effectiveness of their wound treatment system, achieving a striking 5-fold reduction in blood loss and a 3-fold reduction in clotting time. In addition, this unique haemostatic hydrogel can form rapid and stable blood clots even in the presence of blood thinners.
With such promising initial results, this revolutionary product has been awarded funding from the US Department of Defense, to undertake preclinical evaluations to gather more data on the safety and efficacy of this agent. The team can envisage a near future in which their wound management hydrogel will become a standard component in first aid kits and soldiers’ packs, enabling bystanders or the wounded themselves to rapidly stop bleeding, improving patient outcomes and, in the end, saving more lives.
